Introduced By Professor Adam Fox and Dr Marie-Therese (Terri) Lovis
This page and the MAP guideline are intended for healthcare professionals. If you are not a healthcare professional, but are concerned that your baby may have Cows’ Milk Allergy, please seek the advice of your GP. GPs have to be aware of so many topics, please feel able to share this website, including the MAP 2019 update with your GP if you feel it could help them to help you.
GPIFN Statement of Introduction:
GPIFN and the MAP guideline team began a conversation around breastfeeding and milk allergy in 2018, following criticism around the messaging relating to breastmilk in the guideline and the potential for over-diagnosis of cows’ milk allergy (CMA). The MAP team were open to dialogue and collaboration, which led to Dr Lovis joining them to work alongside representatives from the Cows’ Milk Allergy Support group. Together, they updated the algorithms and produced a patient leaflet supporting the need to protect breastfeeding and striving to avoid over-diagnosis, highlighting that common infant feeding issues can have a similar presentation to CMA.
In the initial dialogue, the MAP team explained that their guidelines have never received any funding either directly or indirectly from any sources and specifically not from any commercial interests. The guideline had been deliberately published as an open access article, to provide full and free access by all healthcare professionals, but as a consequence of this, there was no barrier to commercial parties using the guidelines as part of promotional material, with their own logos on. This had led many to assume that the guidelines had been funded by or developed in partnership with the manufacturers of hypoallergenic infant formulae.
GPIFN and the MAP team have shared goals of promoting appropriate management of infants with suspected milk allergy, avoiding over diagnosis or delayed diagnosis, encouraging breastfeeding and improving the quality of life for families and infants. We welcome the changes in the new 2019 MAP Guidelines that protect breastfeeding and aim to avoid over diagnosis whilst at the same time aiding early and correct diagnosis of CMA to avoid unnecessary suffering of infants and their caregivers.
These guidelines were developed, published and remain free from any form of industry support – financial or otherwise for the MAP or GPIFN teams. The MAP guidelines have been again released as an open source publication, but for clarification: If this MAP 2019 guideline is reproduced outside of the GPIFN website or the original publication, particularly by commercial interests, it is without the knowledge or consent of GPIFN or the MAP team.
A Message from the Authors of MAP/iMAP Guidelines
As the authors of the MAP guidance (2013), which has since been replaced by the iMAP guidance (2017) and more recently updated in 2019, we wanted to highlight some important points.
The various iterations of the MAP guidelines were developed by the consensus expert opinion of 13 international clinicians each with a special interest in milk allergy as well as patient input. These MAP guidelines are published in open access, peer reviewed, scientific journals, which allows for maximum access, but also means permission is not required to reproduce them and so these guidelines have been reproduced in the past by commercial interests without approval by the iMAP team.
The motivation for producing the guidance was the reported delayed diagnosis of non IgE mediated milk allergy. Many of the authors were involved in the 2011 NICE Guideline for Assessment and Diagnosis of Food Allergy and thought that a more specific UK, primary care focussed, guideline for delayed-type milk allergy could make a real difference to reduce this delay and thus reduce unnecessary suffering of infants and their carers. It is just as important not to overdiagnose CMA, as this may have important consequences too.
We have asked the GPIFN, to host the iMAP guideline, which they have kindly agreed to do without charge, to allow us to update it over time and provide useful accompanying resources.
Cows’ Milk Allergy & Using the MAP Guidelines (2019)
In using the MAP guidelines, it is critical to remember that milk allergy affects less than 2% of UK infants. Diagnosis is a particular challenge as most of the typical symptoms are very common in well babies – in fact, most babies will suffer from these symptoms from time to time and of course, the overwhelming majority do not have a milk allergy and do not need further assessment for this. However, in infants where these symptoms are multiple, significant, persistent as well resistant to medical treatment, it is important to consider this diagnosis.
At this point, clinical judgement, together with discussion with parents, is required to decide if a diagnostic milk exclusion is warranted. Please note, a cows’ milk exclusion trial MUST be followed by reintroduction of cows’ milk, if the diagnosis is to be confirmed or excluded. This is now a NICE Quality Standard and failure to do this will lead to unnecessary over-diagnosis.
It is also essential to use every possible opportunity to promote breastfeeding amongst the mothers of infants suspected of milk allergy and we have produced a new information leaflet to aid this. WHO guidance is to breastfeed exclusively until 6 months of age and to continue to breastfeed until at least 2 years of age. The benefits of breastfeeding up to and beyond 2 years have been detailed in an excellent Lancet series here . Mothers should be supported to breastfeed as long as they wish to and this support can be particularly important when mothers are following a dairy free diet. The increase in vegan foods available means that there is an ever growing choice of dairy free and tasty foods available for mothers. There are links below that mothers may find useful.
Breastfeeding mothers of infants with CMA should be referred alongside their infant to a paediatric dietitian for advice about their own diet. Please do not advise a mother to stop breastfeeding on the basis of a diagnosis of CMA. Your encouragement can help her to continue for as long as she wishes to.
Evidence based summaries of formula milks can be found here. Primary Care Clinicians should consult their local guidance about preferred prescription milks if required for formula fed infants. In a well infant with an otherwise varied diet most children can be moved from prescription formula onto widely available dairy free milks at the age of 1. It is important to remember that children under 4.5 years should not be given rice milk and replacement milks should be fortified with 120mg calcium: parents should be encouraged to check this when buying from the supermarket. These milks are usually found in the UHT aisle at supermarkets.
Background to the MAP
The Milk Allergy in Primary (MAP) Care guideline was first published in 2013. MAP aimed to provide simple and accessible algorithms for UK clinicians in primary care, detailing all the steps between initial presentation of Cows’ Milk Allergy (CMA), through diagnosis, management and tolerance development. It was developed by the clinicians who had been involved in the development of the 2011 NICE Assessment and Diagnosis of Food Allergy in Children (CG116) without any funding support and published in Clinical & Translational Allergy, an open access journal of EAACI.
The UK Department of Health subsequently commissioned NICE to produce several important publications related to the better recognition, diagnosis and management of food allergy and in particular CMA:
2015 – Clinical Knowledge Summary (CKS) on managing cows’ milk allergy in children, signposting to MAP in order to guide on the management of mild-to-moderate Non-IgE mediated milk allergy in primary care settings
2016 – Quality Standard for food allergy in children.
Despite its UK focus, it soon became clear that MAP was being accessed internationally and thus an updated iMAP (International Milk Allergy in Primary care) guideline was published in 2017, with 7 additional expert international authors from Asia, Africa, Australia and the United States. Both guidelines used existing international consensus guidelines to develop accessible algorithms accompanied by patient information leaflets with updated information from the NICE guidelines and recipes altered to meet WHO standards and aims regards reducing refined sugar and salt intake.
In 2018, the guidelines were criticised for 3 distinct reasons: promoting the overdiagnosis of cows’ milk allergy (CMA), negatively impacting breastfeeding and the possibility of industry influence on the guidelines. The authors addressed these criticisms in a further 2019 update of MAP, using available evidence and, in the context of this and in consultation with patient groups, members of the General Practice Infant Feeding Network and other infant feeding healthcare leads, have collaboratively produced updated algorithms and an information leaflet to support breastfeeding.
This MAP guideline update was published in Clinical & Translational Allergy in 2019 and is available for download directly from their website here.
We believe iMAP is now closer to its original aim of facilitating early and accurate diagnosis of CMA, whilst minimising, as far as possible, any concerns around overdiagnosis or a risk to breastfeeding rates. We continue to welcome open and constructive engagement about how best to achieve these aims to provide evidence-based, practical guidelines for the primary care practitioner.
The MAP Guideline 2019 and Resources
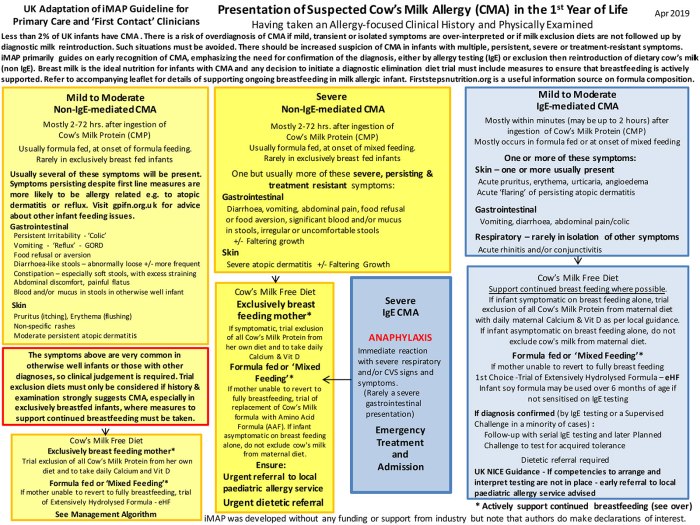
The updated MAP guideline (2019) is still focussed on 2 algorithms.
- Setting out all the possible clinical presentations.
- Guidance on which presentations should be referred on.
- Guidance on which form of diet all suspected infants need to be started on.
iMAP treatment algorithm– for mild-to-moderate suspected non-IgE CMA only i.e. those patients most commonly seen and who can be managed in primary care
- Clinically distinguishing between the exclusively breast fed and the mixed or formula fed.
- The initial diagnostic Elimination-Reintroduction dietary exclusion trial to confirm or exclude the diagnosis.
- When referral for dietetic support is advised.
- When and how to test for later naturally reacquired tolerance to milk protein.
Supporting Tools for the iMAP Algorithms
Allergy-focused History The key questions that need to be addressed when milk allergy is suspected.
Healthcare Professional Factsheet A clinician’s guide to using the iMAP guideline.
Patient Factsheet for infants suspected of having delayed type CMA To explain the diagnosis and the need to confirm it with a planned reintroduction at home.
NEW – supplementary Patient Factsheet for infants with symptoms of a possible mild to moderate non-IgE mediated allergy whilst being exclusively or partly breastfed To support a return to breastfeeding, as the optimal management for CMA.
Home Reintroduction Protocol to Confirm or Exclude Diagnosis The practical details for the family of how to carry out the reintroduction at home.
iMAP Milk Ladder The practical details of testing for naturally reacquired tolerance to milk protein with time.
iMAP Published Recipes The published practical details with regard to the baking/preparing of each Step of the Milk Ladder at home.
Additionally – The Recipes for Steps 1, 2 and 3 have also been set out in a more user-friendly format for bakers at home to follow:
- UK Home Recipe Sheet 1 – Biscuit (found here)
- UK Home Recipe Sheet 2 – Muffin (found here)
- UK Home Recipe Sheet 3 – Pancake (found here)
The full earlier 2017 iMAP paper can be downloaded directly from the journal website here. iMAP includes:
- All the essential advice within the recent UK NICE publications.
- Amendments to reflect the constructive feedback received from the increasing use of MAP in the UK.
- It continued to be set out in 2 key easy to follow algorithms.
- Updated milk ladder with new recipes that comply with the World Health Organization recommendations for refined sugar and salt content.
- Practical Guidance Sheets on CMA.
NON iMAP USEFUL RESOURCES FOR CMA INFANTS AND THEIR FAMILIES
GPIFN and IMAP do not have control over the following links but patients have given feedback that they found them useful so we include them as a popular resource to aid you in providing holistic care to your patient.
- Dilan and Me Hints and tips for breastfeeding a baby with CMA (non NHS site but very useful practical advice for mothers).
- First Steps Nutrition Trust: Eating Well for Infants and New Mums Nutrition guidance on vegan diets for the under 5s.
- British Dietetics Association: Milk Allergy guidance on a dairy free diet and advice on food labels and on the best dairy free substitutes for particular uses including the morning coffee.
- British Dietetics Association: Food Fact Sheet Calcium Guidance on sources of calcium.
- First Steps Nutrition Trust: Infant Milks Information for Health Workers Nutrition guidance on infant formulas
- When it isn’t CMA… support for parents to help them understand ‘colic‘ and the exhausting phase sometimes known as ‘purple crying‘.
- A useful evidence based resource to provide information on infant sleep including reassuring parents that it is normal for infants to wake at night.
Resources for the Breastfeeding Mother
Associations that can further support breastfeeding:
There are many sources of support to help your patient to continue breastfeeding for as long as she wants to.
Some of these are listed below.
- Local NHS Breastfeeding support service (details in your baby’s red book) – a good first stop.
- Breastfeeding support telephone lines:
- National Breastfeeding Helpline – 0300 100 0212.
- Association of Breastfeeding Mothers – 0300 330 5453.
- National Childbirth Trust (NCT) – 0300 330 0700.
- La Leche League (0345 120 2918) provides very useful information on breastfeeding on their website, you can find a local group that may be able to also support you. http://www.laleche.org.uk
- The Breastfeeding Network provides support for breastfeeding provide telephone support. Importantly they also have useful prescribing guides for healthcare professionals prescribing for breastfeeding mothers
https://www.breastfeedingnetwork.org.uk/breastfeeding-support/ - Breastfeeding support group for children with cows’ milk allergy https://www.facebook.com/groups/CMPASforBreastFeeding/
- The NHS also has support websites – https://www.nhs.uk/conditions/pregnancy-and-baby/benefits-breastfeeding/
and https://www.nhs.uk/conditions/pregnancy-and-baby/problems-breastfeeding/ - GPs can access information on http://www.gpifn.org.uk
- First Steps Nutrition – https://www.firststepsnutrition.org/eating-well-infants-new-mums
- Start4Life Breastfeeding Friend – an NHS supported Facebook group that offers advice day or night.
Meet the Team
Find out more about and contact the MAP team here.
Published 5th October 2019, Updated 7th October 2019


You must be logged in to post a comment.